I am a doctor and this covid symptom me the most scar
What it means, and how to treat it.

Of all the unpleasant symptoms I have attended as a doctor, the one I fear the most is shortness of breath, sometimes calledshortness of breath. It's aCommon symptom of COVID-19And in this article, I will tell you how to recognize it and what to do if you do it. Read on and ensure your health and health of others, do not miss theseWithout signs that you have already had coronavirus.
What should it be like to experience acute and severe acoustic breathing? When I try to imagine this, I think of how it feels when you dive into a pool and swim towards the surface, desperately want to take a breath. There is a sense of effective anticipatory anticipation of the need to take a breath - a kind of brilliant feeling in your chest. It only time lasts for seconds, because when you break through the surface of the water, you take a huge air stupil and that you instantly have a feeling of need to breathe.
But imagine if you have felt like most of the time - for example, if you had severe Covid pneumonia? Each breath you manage to take can not end the desperate feeling. It is absolutely, unimaginably painful.
If you ask people who had acute acute acute attack, they will tell you that being unable to breathe is the most frightening thing they have ever experienced. People often describe the fear and anxiety that comes with a feeling of imminent misfortune, that something terrible is about to happen.
These are the most important things to know about the breathlessness of Covid, how to deal with it, and when it is a medical emergency.
Normal respiratory rate

All of usto breatheregularly, inside, without thinking about it. We vary our breathing unconsciously all day, when we talk, eat and drink, or maybe to stop breathing in a big cloud of exhaust fumes.
We generally only take awareness of our breathing if something is wrong, and we start to feel out of breath. The term medical for shortness of breath is dyspnea.
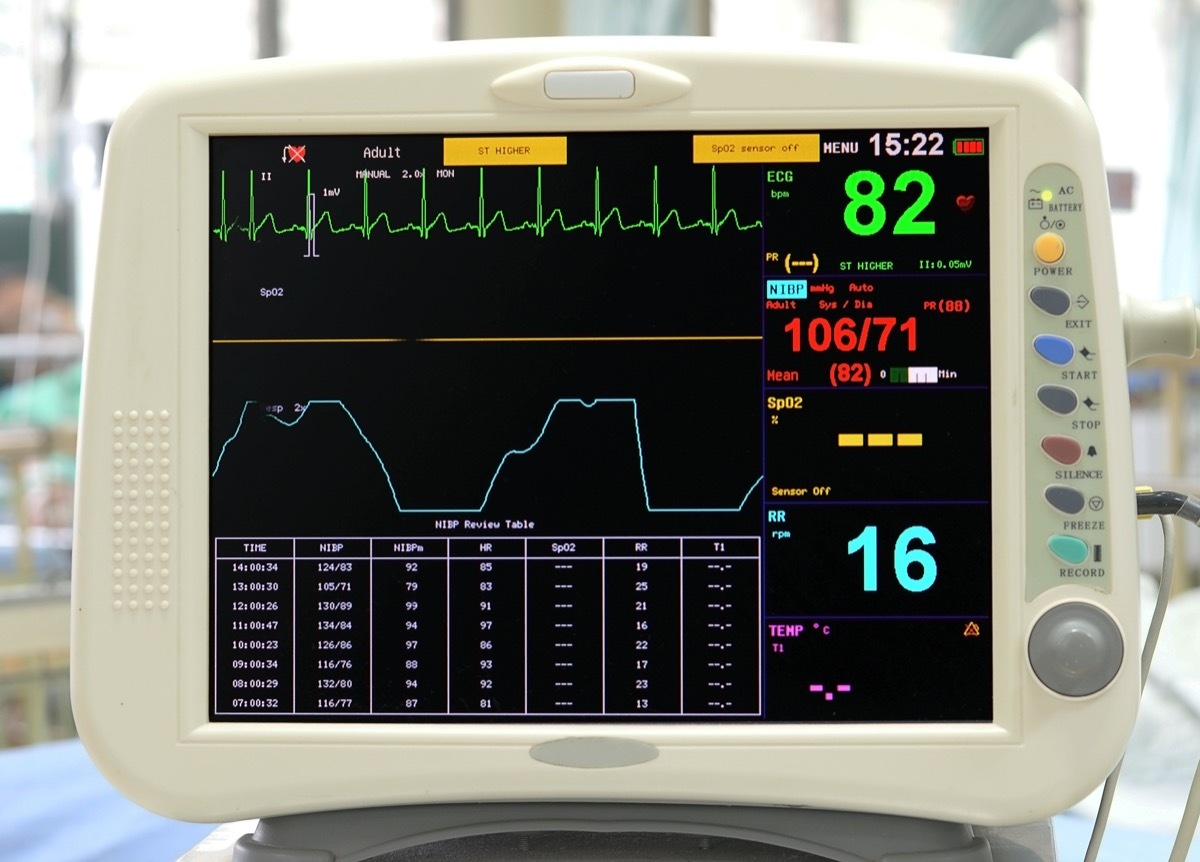
- Therespiratory rateis one of our four vital signs (pulse rate, blood pressure, respiratory rate and body temperature).
- The respiratory rate is the number of times we breathe every minute, at rest.
- For an adult, a normal respiratory rate is 12 to 16 breaths per minute.
The importance of our vital signs
Our bodies are like any well oiled machine. As long as all parts of the body and organs are in good working order, everything is fine. But if something emphasizes the mechanics, a part of the body (or an organ) fails, the machine is wavering and these vital signs become disturbed. If you go to the sick doctor, so they check for the first time these four vital signs looking for a motor failure.
We have to breathe to stay alive

Breathing is essential for human beings to be alive. When we breathe, oxygen goes into our lungs and diffuses through tiny capillaries in the blood. At the same time, carbon dioxide is evolving from these capillaries and in the lungs, and we breathe that. This transfer of gas takes place continuously in tiny and aerial bags in the lungs, called alveoli.
What causes shortness of breath?

If something disturbs this transfer of gas, your brain notes there is less oxygen on board and tells your body to breathe faster and to raise these oxygen levels as soon as possible. Your brain continues to tell your body to do so until the supply of reduced oxygen has been corrected.
If you are out of breath because you ran for a bus, the feeling out of breath will disappear shortly after you are on the bus and you sit down. But if you feel out of breath because of Covid-19 pneumonia, feels a lot longer, sometimes for several weeks.
Many things disturb the transfer of gas into the lungs. Here are some common examples:
- Infection. For example, Covid-19 causes pneumonia, resulting in fluid buildup in the cells. The presence of this fluid reduces the efficiency of oxygen and carbon dioxide transfer.
- Respiratory conditions, such as asthma, cause bronchioles (pulmonary tubes) to contract and reduce, which means that sufficient air can be physically in the lungs.
- In COPD, the lungs are damaged by smoking and filling tar and mucus cells.
- Other medical conditions can cause fibrosis in lung tissue, which means that the lungs are stiff and can not develop and contract appropriately.
- If your blood circulation is compromised, for example, low blood volumes, dehydration or shock - it can also cause shortness of breath.
What happens when you are infected by Covid-19?

Imagine today was the day you were infected with Covid-19. Maybe you without knowing a metro car with an infected person, the virus that was also excretion without knowing it. In a way that you jostled for a seat and sitting for about 15 minutes, you managed to breathe enough viral particles to be infected.
These tiny virus particles penetrate in the cells that light the respiratory tract: the mouth, nasal ways and respiratory tract. Once they enter your cells, they reproduce, creating many viral particles that propagate more throughout your body. You are now excreting the virus when you exhale, cough or sneeze, and can infect someone else nearby.
It seems incredible that despite all this happens, a huge 80% of people with COVID do not have any symptoms and do not know they have. But that seems to be the case. This is a trick of a virus- smart if a virus wants to succeed, it must work in Catimini and do not get caught!
So all these new virus fees can now be transmitted as breathing droplets when you exhale the air, or when you cough or sneeze. They can also survive on infected surfaces, including your inanimate hands and objects such as worktops, kitchen equipment, and toilet seats. That's why cover your nose and mouth with a mask, wash your hands frequently, and keep your home and bathrooms clean, are essential to prevent you from infecting someone else inadvertently.
A positive Covid person can infect up to403others over a period of 30 days. However, if social distancing and infection control measures are followed as above, which reduces the risk of transmission of more than 95%-for only 2.5 people contract the infection.
It's not as simple as having a COVID test. As strange as it may seem, in an early infection of a COVID antigen test can be negative.
COVID-19 SYMPTOMS-ALL COMMENT DEVELOPMENT

The symptoms of the most Covid-19 infection are fever and a dry cough. However, 5% to 60% of COVID patients complain about breathing difficulties. This tends to together betweenday and four days 10. Not everyone with Covid gets out of breath, but for those who do it, it's a bad predicted sign.
Why does Covid-19 go out of breath? The virus causes pneumonia. As the virus spreads in your lower respiratory tract, your pulmonary tissues become inflamed. There is an accumulation of inflammatory liquid in tiny air pockets called pulmonary cells. The presence of this fluid prevents the diffusion of oxygen from the lungs and in the blood, which means that your oxygen saturation begins to fall.
As soon as the brain recognizes these levels of oxygen fall, you breathe faster and deeper, to attract more air into your lungs. This now seems difficult to breathe. Over time, if you still have not developed sufficient antibodies to erase the virus, your respiratory rate can continue to increase. You may notice that you feel out of breath at just sitting on a chair and all your usual activities are difficult or impossible. You can not walk away, and you probably can not handle the stairs. If your symptoms are as bad as that, it is an emergency.
In severe acute Covid, intensive admission is generally recommended if oxygen saturation is less than 93%, and / or your respiratory frequency greater than 30 respirations per minute.
Who could be at risk of dyspnea with COVID?

Many individualsrisk factorsYou put at a higher risk of serious COVID-19 infection. Many of them are either medical conditions or lifestyle factors that put your respiratory function under additional pressure. For example:
- A more advanced age. Your immune system is less effective than you get older.
- Chronic pulmonary conditions for example. Asthma, chronic obstructive pulmonary disease (COPD), emphysema, chronic bronchitis, alter the lung function.
- Cardiopathy. Allcardiac problem, Like angina of chest, a heart attack or heart failure, means that you are more at risk of Covid Serious infection -19.
- Diabetes. High blood sugars increase the risk of COVID-19. UncontrolledDiabetesdoubles your death risk.
- Arterial hypertension. More COVID-19 deaths appear to occur in patients withHypertensionBut if it is directly due to high blood pressure itself, or if it is due to other medical conditions often associated with arterial hypertension is still unknown.
- Smoking.SmokersRun a greater risk of serious COVID-19 infection than non-smokers.
- Kidney disease. A recent United States2020Meta-analysis concluded that the risk of severe Covid-19 infection in people with chronic renal disease is three times higher.
- Liver disease. People withliver diseaseSuch as cirrhosis, foie gras, hepatocellular carcinoma and liver transplants are also at increased risk of severe Covid-19 infection.
- Neurological disease. There seems to be a link between an increased risk of death of a serious COVID infection anddementiaas well as other neurological conditions such as stroke.
- A weakening of the immune system. There have been several cases of cases of severe CIVID-19 infections in patients with organ transplant and with various types of autoimmune diseases. The exact risk posed by a sub-assetimmune systemNot well understood, but anyone with a compromised immune system is currently considered a higher risk of CIVID-19 infection.
- Obesity. UKData analysisShows that two-thirds of patients admitted to the ICU with serious COVID-19 were overweight or obese.
- Bame (black and minority ethnic groups) groups. It is not clear why people of BAMES are more at risk of COVID-19, but this may be due to a combination of factors, including factors such as deprivation, housing unclogped and / or type d 'use. Studies are underway to learn more.
- Your job. The risk of infection is COVID three times higher among front-line medical care staff, despite the use of PPE. A July 2020 studyThe lancetReported 2,747 COVID cases per 100,000 people in health staff, compared to 242 per 100,000 for the general population. The calculation has been adjusted because health care staff is more likely than the general public to be tested. However, even after being adjusted for that, they were always three times more likely to become infected.
Live with a COVID-19 infection

It can be difficult to know when to call with a COVID infection. After all, when you test positive, you are quite told firmly to stay at home. However, remember:
- 4 out of 5 patients only have a slight infection.
- 80% of people with COVID have no symptoms, or just very light symptoms.
- Covid-19 is a virus, so antibiotics do not work.
- It is a question of rest, fluids, and let the time pass so that your body can develop antibodies and get rid of the virus.
You need to stay at home andself-isolationFor at least 10 days after the appearance of your symptoms. After that, if you just have a cough and a loss of sense of taste or smell, you can stop isolating yourself out, but if you have other symptoms, you should continue to isolate themselves up to whatsoever party. here's howisolate.
Everyone in your home should also be isolated for 14 days from the day you had symptoms.
However, for some patients, symptoms can be unpleasant and severe. One of these miserable symptoms is out of breath feeling.
What do we know about Covid-19 and feel out of breath?

If the symptoms of COVID develop, it is usually about five days after being infected. The majority of people with symptoms complain about fever and cough. Shortness of breath is only present in31% to 40%Persons with happening.
The degree of dyspnea can be light, moderate or severe. Your condition can deteriorate quickly, sometimes in a few hours or minutes.
In the majority of people, the feeling of breaths will improve your body develops antibodies and fights against infection. However, in small fewer people, this may worsen, which requires admission to the hospital and / or intensive care treatment. In the most severe cases, a mechanical fan is needed to take breathing.
The overall risk of death of a Covid infection is pretty much1.4%. The risk increases with the growing age: 1 of 300 under 60, 1 out of 16 over 60 and 1 over 7 over 80 years old.
When shortness of breath is an emergency?

If you are extremely breathless, it's a medical emergency. If you have one of the following signs, you or a guard mustcall 911without delay.
- Be unable to finish a sentence without breathtaking
- Be unable to speak
- To be unable to do normal things like the bathroom on foot or handle the stairs
- Feeling confused, or disoriented
- You are afraid of your breathing / inability to breathe
- Developing new symptoms such as chest pain or the quasihood of blood / blood stained sputum
How can you evaluate your own breathing?

It is virtually impossible to properly evaluate your own breathing, especially if your symptoms are serious. If you are worried at all, it is better to get an urgent medical assessment and not to wait.
"Happy hypoxemia"

One of the strange things about COVID infection is that infected patients may not fully realize how breathable they are.
To feel out of breath, your brain must recognize the situation and send an alert. But in a COVID infection, unclear reasons, this mechanism is blunt. This led to a term- "Happy hypoxemia"-Mans often, Covid patients are very out of breath but are not aware of the severity of their condition.
As a result, it takes more time for them or their guardians to appreciate how bad they are sick and leads to a delay in access to the hospital.
Do not take risks. If you are concerned about your breathing, get an appropriate medical assessment without delay.
How can doctors assess your breath?

Doctors are often faced with having to assess your condition on a video link. They must have simple ways to judge how your breathing is affected. Sometimes they use an algorithm called theRoth score. That's how it works.
You are asked to take a breath and count until slowly aloud. The doctor will have time for how long it takes before taking a breath when reciting numbers. If it has less than 8 seconds, your oxygen saturation will probably be less than 95%. If it's within 5 seconds, your oxygen saturation is likely to be less than 91%.
In fact, the Roth score is not so precise. The main problem is that it can give you pleasure to advise you to go to the hospital too often. However, it's a convenient and simple way for you to get an idea of the severity of your breathing.
Questions "Red Flag"

It is also important to keep tabs on how things change. What can not you do today that you could do yesterday?
How would you answer the following questions?
- Are you so out of breath that you are unable to speak more than a few words?
- Do you breathe stronger or faster than usual doing nothing at all?
- Are you so sick that you have stopped doing all your usual daily activities?
If the answer to one or more of these questions is "Yes", you need urgent medical help.
Other signs of respiratory difficulty

You can say that people have difficulty breathing by observing the following clinical signs and features. People who can not breathe well, must work hard at their breathing.
They often
- Sit straight and can not go back to their pillows or stay flat in bed
- Hold the table in front of them or for example a pillow stack, as they have trouble breathing
- Use additional muscles to breathe, such as their neck muscles
- Use their diaphragms to breathe, so you can see the abdomen move and go out with each breath
- Have flared nostrils while they try to suck more air in their nasal passages
- Have difficulty eating and drinking because they can not risk interrupting their breathing
- Can not communicate, as they can not listen to or speak, and can be agitated and irritable as their breathing takes up everything
- Can be disoriented and not know the day or time, or be confused
- May not be able to take their usual medicines
- Their lips may seem thin and blue, and their fingers and their fingers may seem blue - it is a cyanosis that occurs when oxygen saturation levels are low.
- Have a tremor. If they hold hands directly in front of them with extended cuffs, a swing tremor can be seen, which is a sign of metabolic disturbance due to the conservation of carbon dioxide.
- Can have sporadic muscle shaking or contractions.
- Can have cold hands and feet.
What can you do to help relieve the symptoms of shortness of breath?
The best way to improve shortness of breath is to treat the underlying cause. But for Covid-19, which is a virus, there is still no effective treatment. Simply wait for your body to produce antibodies to kill the virus.
However, some things can be done to help support breathing and help relieve the feeling of shortness of breath.
- Sit up. A chair can be better than a bed. Sit forward and have something in front of you to rest your hands.
- Try to stay calm. It's easier said than doing, but anxiety aggravates breathing. Try to breathe deeply and slowly. Entering a pace: Breathing the count of one, and as you count 2 and 3. It is always important to breathe longer than you breathe. Remember that you need to expel your lungs to get room for room to get more air in, so that breathing is an important part of the process. If you do not breathe completely, you will keep more carbon dioxide. Make sure you are not just panting, with short fast breaths, as it is counterproductive.
- Actively use your diaphragm to breathe. Remember to lift your thoracic cage when you breathe, lifting the midrift up. You can see and feel your belly move and go out when you do it correctly.
- Some people find the pursuit of their lips when they expire help. This is because you empty your lungs better when you breathe against forced resistance.
- Keep the window open or sit down by a door. Fresh air however helps with COVID the use of fans is not allowed because of the increased risk of spreading infection.
- Keep hydrated. You need a good volume of blood to maintain good blood circulation. Have Gengments, little and often.
- Take your regular medicine. This includes all inhalers or nebulizers that you usually use.
- Steam inhalations can help loosen mucuses and soothe inflamed respiratory tract. Vicks or other steam friction can be useful. Try a hot shower.
- Use a home humidifier.Researchshowed that the virus spreads faster under dry environmental conditions. When the air is dry, the mucus is thicker and the small cells the lining of the respiratory tract are less good at the mobile mucus up and away from the lungs. TheCDCRecommends the use of a humidifier to treat COVID. Aim about 50% moisture from the air. You can do it just having a saucepan of boiling soft water in the room. Or by buying ahumidifier.
Chest Exercises

Have you heard of Huff?
When youto blowI think of what you do when you polish a mirror. Breathe hard and quickly, one or twice. To do this, you suddenly contract your chest and stomach muscles. This can bring a cough fighting as you will loosen thoracic secretions - which is good.
Do this for about 10 minutes, two to three times a day. Stop doing it when you have done the Huff cycle twice, but do not fear any mucus.
Sleep positions

Sleep can be difficult if lying brings your cough and makes breathless worse. Only do what feels possible. In principle, you must move and change the position of your chest to drain all lobes from the lungs. So when you sleep, try using pillows to accompany you on one side, then on the other side, even down a little, even for short periods to encourage fluid and mucus in your lungs to move .
Oxygen therapy

Your oxygen saturation level will determine if you need additional oxygen. In general, you need oxygen if your oxygen saturation is less than92%But this threshold is sometimes lowered if you have other chronic diseases. This is simply measured using a device called apulse oximeter.
- OxygenThe gas is provided via a facial mask for you breathe, at the hospital. However, if you simply breathe more oxygen does not improve your oxygen levels, the CPAP can be tried.
- Pressure Respiratory Pressure Pressure Continuous (CPAP)- This means that oxygen is from the blowing in your lungs under pressure. Although this is often effective, there is an increased risk of transmitting the virus to other health workers, and the staff needs very effective EPP.
- Mechanical ventilation- It means that you are in sedation and the machine takes breath for you. It's a high-risk situation. About 33% of those ventilated for a COVID infection recovered.
Practical support

One way to feel less pushed is to reduce the requirements on your body. The least active you can be with your home tasks, the more energy is left on you to focus on breathing and give your body time to recover. It means thinking about a personal organization. You may need someone to help you.
- Shop once a week, online if possible, and get home delivery rather than missing things every day.
- Buy simple prepared foods that do not need a lot of effort to cook.
- Keep everything at your fingertips, so you do not need to reach high shelves or search closets.
- Accept the help of friends, families and neighbors. They can walk on the dog and water your garden. Keep your energy to do well.
- Keep a list of important numbers next to your phone. Have also programmed them in your phone, so it's easy to ask for help.
- Pace yourself during the day. Accept that things will take more time - do not rush. You have time to breathe calmly and pass through every day the best you can.
- It's good to feel tired. The disease is exhausting. Rest is important for healing. You do not feel bad not to be able to do anything. Sitting quietly, breathe and distract from television or music.
- Eating for health. Eat small feeding portions of food to support your immune system and give you energy.
To stay positive

Many people living in the pandemic find theirMental Healthis not good right now. If you are infected with COVID, this brings a range of pressures, anxiety and restrictions, and it is likely to emphasize even more your mental health.
Try to stay calm and positive. Anxiety and stress affect the immune response. Tell yourself firmly that you fight this infection and carefully follow all the advice.
Think about the right points:
- Although Covid is a serious infection, about 99% of people survive.
- Those who have the most serious infections seem to have the best antibody response.
- Only confidence visits resources such as government or charitable sites for reliable information. Do not be fooled or getting and worried about false news.
- Do not listen to the news too often. A constant deluge of sensationalist stories does not allow. Listen to music or read a book instead.
- Stay in touch with friends and family. Although you are probably going to be self-insulating, you can have phone and video calls with your friends and family. Its very important.
- TheCDChas published a list of telephone resources and permanence.
As for yourself: go through this pandemic at your healthier, do not miss these35 places you are most likely to catch Covid.

The former teenager star reveals how much she really won - and how she lost millions

